Creating Optimal Member Engagement While Delivering Compliant Outcomes & Financial Results
Improve engagement and attain compliant financial results.


Empowering Your Organization for Success
Maintain compliance with tech-enabled, cost-effective resources aimed at generating accurate and complete results
Achieving compliant and optimal financial results requires successfully navigating the complex and evolving regulatory requirements associated with Medicare Advantage, Medicaid, and Commercial ACA.
Omega Healthcare simplifies the process with intelligent, industry-leading, end-to-end tech-enabled solutions. We provide the tools you need to strengthen member/provider engagement for optimal outcomes and financial results.
800
Risk adjustment coding and HEDIS abstraction specialists
60%
Estimated savings on each HCC medical chart review and/or HEDIS abstraction
98%
Coding accuracy

Value-based care
Communicate with providers and members in a way to support clinical outcomes and member satisfaction.

Risk management & quality improvement
Ensure compliant HCC capture and optimize source data quality for accurate HEDIS and Star reporting.

Administrative Support
Streamline processes for membership management, provider network and data management, and claims auditing.

Outcome
Payers operate with greater efficiency and foster meaningful connections with members and providers.
Intelligent Payer
Operations Solutions
Value-based Care
We facilitate compliant and optimal financial results for risk adjustment and quality of care across all manner of engagement models (i.e., prospective, concurrent, and retrospective).
- Risk Adjustment Documentation and Coding Review
- HEDIS Chart Abstraction
Provider & Member Engagement
We provide resources to support your provider and member interaction needs, including health monitoring, provider outreach, and more.
- Care Coordination
- Provider & Member Communication
- Utilization Management
Administrative Support
Our team provides claims processing support and coordinates administrative tasks like credentialing while identifying opportunities to increase utilization within your network.
- Claims Administration
- Member Management
- Provider Data & Network Management
Contact Us
Contact us today to learn how our technology-led, clinically enabled solutions can help your organization thrive.
Who We Help
Payers
We are a leading provider of tech-enabled solutions for entities with commercial ACA, Medicaid, and Medicare Advantage lines of business.
- Commercial ACA
- Medicare Advantage
- Managed Medicaid
- Payviders and Risk-bearing Entities
- Channel Partners
Contact Us
Contact us today to learn how our technology-led, clinically enabled solutions can help your organization thrive.

Featured white paper
Best Practices to Achieve HCC Compliance
Uncover strategies for payers to enhance HCC coding accuracy, improve reimbursement, and optimize health outcomes.
The Latest News from Omega Healthcare
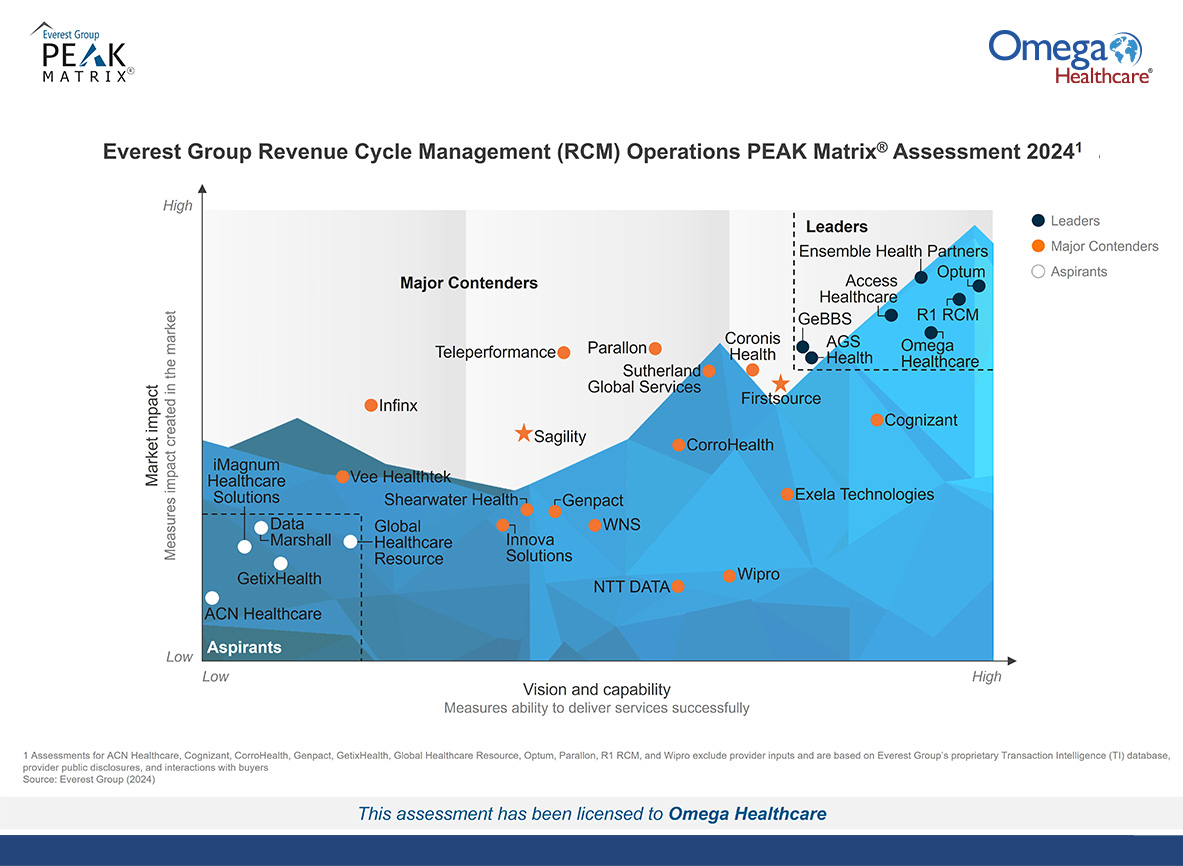
Omega Healthcare Named a Leader in the Everest Group Revenue Cycle Management (RCM) Operations PEAK Matrix® Assessment, 2024
The Leader designation reflects Omega Healthcare’s differentiated technology innovation, partnership...
Read MoreOmega Healthcare Processes 60 Million Transactions with Enterprise AI and Automation from UiPath
NEW YORK, NY and BOCA RATON, Fla., Oct. 23, 2024...
Read MoreOmega Healthcare Named Horizon Three Market Leader in HFS Horizons: HCP Service Providers, 2024 report
HFS Research recognizes Omega Healthcare’s rapid transformation to tech-enabled partner...
Read MoreOmega Healthcare Named a Leader in the Everest Group Revenue Cycle Management (RCM) Operations PEAK Matrix® Assessment, 2024
The Leader designation reflects Omega Healthcare’s differentiated technology...
Read MoreOmega Healthcare Processes 60 Million Transactions with Enterprise AI and Automation from UiPath
NEW YORK, NY and BOCA RATON, Fla., Oct....
Read MoreOmega Healthcare Named Horizon Three Market Leader in HFS Horizons: HCP Service Providers, 2024 report
HFS Research recognizes Omega Healthcare’s rapid transformation to...
Read More